Artificial retinas: promising leads towards clearer vision
A major therapeutic challenge, the retinal prostheses that have been under development during the past ten years can enable some blind subjects to perceive light signals, but the image thus restored is still far from being clear. By comparing in rodents the activity of the visual cortex generated artificially by implants against that produced by “natural sight”, scientists from CNRS, CEA, Inserm, AP-HM and Aix-Marseille Université identified two factors that limit the resolution of prostheses. Based on these findings, they were able to improve the precision of prosthetic activation. These multidisciplinary efforts, published on 23 August 2016 in eLife, thus open the way towards further advances in retinal prostheses that will enhance the quality of life of implanted patients.
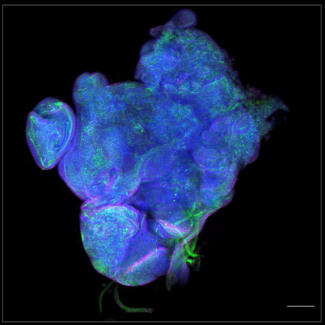
A retinal prosthesis comprises three elements: a camera (inserted in the patient's spectacles), an electronic microcircuit (which transforms data from the camera into an electrical signal) and a matrix of microscopic electrodes (implanted in the eye in contact with the retina). This prosthesis replaces the photoreceptor cells of the retina: like them, it converts visual information into electrical signals which are then transmitted to the brain via the optic nerve. It can treat blindness caused by a degeneration of retinal photoreceptors, on condition that the optical nerve has remained functional1
. Equipped with these implants, patients who were totally blind can recover visual perceptions in the form of light spots, or phosphenes. Unfortunately, at present, the light signals perceived are not clear enough to recognize faces, read or move about independently.
To understand the resolution limits of the image generated by the prosthesis, and to find ways of optimizing the system, the scientists carried out a large-scale experiment on rodents. By combining their skills in ophthalmology and the physiology of vision, they compared the response of the visual system of rodents to both natural visual stimuli and those generated by the prosthesis.
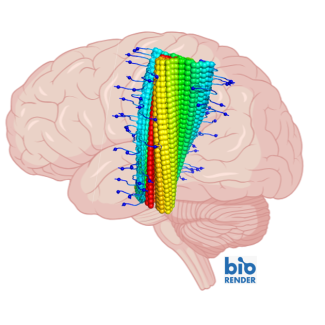
Their work showed that the prosthesis activated the visual cortex of the rodent in the correct position and at ranges comparable to those obtained under natural conditions. However, the extent of the activation was much too great, and its shape was much too elongated. This deformation was due to two separate phenomena observed at the level of the electrode matrix. Firstly, the scientists observed excessive electrical diffusion: the thin layer of liquid situated between the electrode and the retina passively diffused the electrical stimulus to neighboring nerve cells. And secondly, they detected the unwanted activation of retinal fibers situated close to the cells targeted for stimulation.
Armed with these findings, the scientists were able to improve the properties of the interface between the prosthesis and retina, with the help of specialists in interface physics. Together, they were able to generate less diffuse currents and significantly improve artificial activation, and hence the performance of the prosthesis.
This lengthy study, because of the range of parameters covered (to study the different positions, types and intensities of signals) and the surgical problems encountered (in inserting the implant and recording the images generated in the animal's brain) has nevertheless opened the way towards making promising improvements to retinal prostheses for humans.
This work was carried out by scientists from the Institut de Neurosciences de la Timone (CNRS/AMU) and AP-HM, in collaboration with CEA-Leti and the Institut de la Vision (CNRS/Inserm/UPMC).
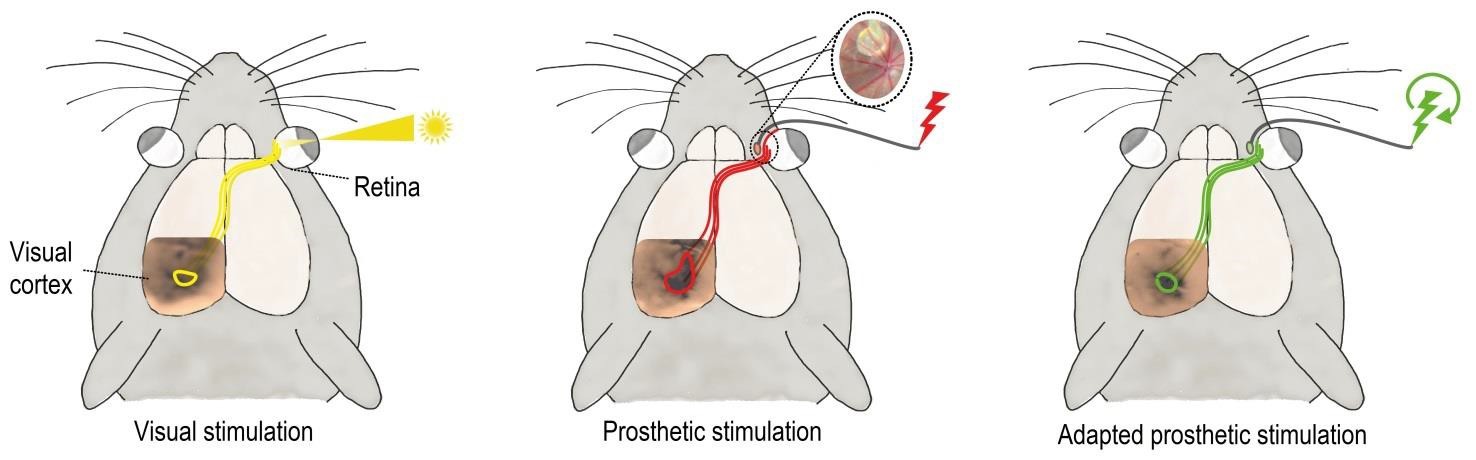
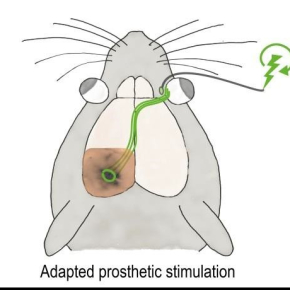
Activation (colored circles at the level of the visual cortex) of the visual system by prosthetic stimulation (in the middle, in red, the insert shows an image of an implanted prosthesis) is greater and more elongated than the activation achieved under natural stimulation (on the left, in yellow). Using a protocol to adapt stimulation (on the right, in green), the size and shape of the activation can be controlled and are more similar to natural visual activation (yellow).
- 1This is the case of patients with Retinitis Pigmentosa or Age-related Macular Degeneration (AMD).
Probing the functional impact of sub-retinal prosthesis. Roux S., Matonti F., Dupont F., Hoffart L., Takerkart S., Picaud S., Pham P., Chavane F. eLife, 23 August 2016.
DOI : View web site